SpiritualFamily.Net
- Activity
- Blogs
- Groups
- Pages
- Newsletters
- Forum
- Study Group Map
- Questions & Answers
- All Groups
- Courses
- 5th Epochal Revelations
- SFN Mission
- 606 NEWS
- Urantia Library
- Urantia Africa
- UB Quotes
- SG Map
- Jesus MeetUp
- EDEN INTERNATIONAL
- DISCIPLESHIP
- Atlanta SG
- JESUS
- Women's Corps
- Citizens in Motion
- Purchase Urantia Book
- Destiny Reservists
- SFN Nexus Hub
- EVERLASTING GOSPEL
- QUORA
- Our Revelation's Digital Path
- DONATE
- More
An Evidence Based Scientific Analysis of Why Masks are Ineffective, Unnecessary, and Harmful PAGE 2 0F 3
An Evidence Based Scientific Analysis of Why Masks are Ineffective, Unnecessary, and Harmful
PAGE 2 OF 3
![]()
The Evidence FOR Masks
The best evidence for masks was commissioned by the WHO and published in the Lancet in June 2020. The title, “Physical Distancing, Face Masks, and Eye Protection to Prevent Person-to-Person Transmission of SARS-CoV-2 and COVID-19: A Systematic Review and Meta-Analysis,” sounds like high-level scientific evidence. After all, systemic reviews and meta-analyses are typically considered the epitome of evidence based medicine. However, don’t be deceived by the authors’ deceptive attempts to elevate the relevancy of this study. This systemic review/meta-analysis was entirely comprised of low-level observational studies. No high-level randomized controlled trials were included.
No matter how much the authors attempt to deceive or embellish the study’s relevance with its “dressed up” title, the fact remains, this study still amounts to nothing more than a steaming pile of weak evidence. No matter how much the authors and the WHO want this study to represent high-level evidence for masking world populations, it simply cannot be considered to be more than the sum of its low level parts.
Furthermore, the study is seriously flawed with serious misrepresentations and misinterpretations of the data. The flaws, errors, and mistakes in this analysis of 29 observational studies should lead to its retraction from the Lancet. The flaws are buried in the data tables, therefore, it is missed by those that do little more than read titles and conclusions. Which is exactly why studies like this should be subjected to thorough and independent peer-review before publication.
Scientists all over the world are raising concerns and speaking against the study and demanding its retraction. For example, University of Toronto epidemiology professor Peter Jueni called the WHO study “methodologically flawed” and “essentially useless”.
Garbage-in-garbage out: the June 2020 WHO commissioned study of masks published in The Lancet.
- Source: Chu, Derek K., Elie A. Akl, Stephanie Duda, Karla Solo, Sally Yaacoub, Holger J. Schünemann, and COVID-19 Systematic Urgent Review Group Effort (SURGE) study authors. 2020. “Physical Distancing, Face Masks, and Eye Protection to Prevent Person-to-Person Transmission of SARS-CoV-2 and COVID-19: A Systematic Review and Meta-Analysis.” The Lancet 395 (10242): 1973–87.
Summary: the WHO-commissioned meta-study on the effectiveness of facemasks and social distancing, published in The Lancet, is seriously flawed and should be retracted.
This study is nothing more than a seriously flawed meta-analysis of 29 weak observational studies. None of the trials were randomized controlled trials. No matter how thoroughly you sift through the weak, low-level of evidence, observational studies, in the end, all you end up with is weak, easily biased, and essentially unusable evidence.
For a more comprehensive analysis of the flaws and a thorough debunking of the relevance of this study, read this: WHO Mask Study Seriously Flawed, Swiss Policy Research (Sept. 9, 2020), copied here:
Update: A US analyst has reviewed all 29 studies and found numerous additional mistakes.
A. General flaws
- Of the 29 studies analyzed by the Lancet meta-study, seven studies are unpublished and non-peer-reviewed observational studies. Non-peer reviewed studies should not be used to guide clinical practice according to the medRxiv disclaimer. [3] [4] [31] [36] [37] [40] [70]
- Of the 29 studies considered by the meta-study, only four are about the SARS-CoV-2 virus; the other 25 studies are about the SARS-1 virus or the MERS virus, both of which have very different transmission characteristics: they were transmitted almost exclusively by severely ill hospitalized patients and not by community transmission.
- Of the four studies relating to the SARS-CoV-2 virus, two were misinterpreted by the Lancet meta-study authors[44] [70], one is inconclusive [37], and one is about N95 (FFP2) respirators and not about medical masks or cloth masks (see detailed analysis below).
- Despite the weakness, misinterpretations, and inapplicability, the Lancet meta-study is used to guide global facemask policy for the general population. However, of the 29 studies considered by the meta-study, only three are classified as relating to a non-health-care (i.e. community) setting. Of these three studies, one is misclassified [50] (relating to masks in a hospital environment), one showed no benefit of facemasks [69], and one is a poorly designed retrospective study about SARS-1 in Beijing based on telephone interviews [74]. None of these studies pertained to SARS-CoV-2.
- The authors of the Lancet meta-study acknowledge that the certainty of the evidence regarding facemasks is “low” as all of the studies are observational and none is a randomized controlled trial (RCT).
- The WHO itself admitted that its updated facemask policy guidelines were based not on new evidence but on “political lobbying”.
B. Study misinterpretations
As mentioned above, several studies have been misinterpreted by the authors of the meta-study. All of the misinterpretations resulted in falsely claiming or exaggerating a benefit of facemasks. In the following, only the four studies relating to SARS-CoV-2 are reviewed. (HCW: health care worker)
- Heinzerling et al. [44]: The meta-study claims that 0 of 31 HCW wearing a facemask and 3 of 6 HCW not wearing a facemask got infected. This is not correct.
The study showed that 0 of 3 HCW wearing a facemask and 3 of 34 HCW not wearing a facemask got infected. This result was not statistically significant (p=0.73). Moreover, of the 3 HCW who got infected, one reported wearing a facemask “most of the time”, but the meta-study classified this HCW as “not wearing a facemask”. - Wang et al. [41]: This study, which did show a benefit of facemasks, was about N95 (FFP2) respirators in a health-care setting, not about medical masks or cloth masks.
- Wang et al. [70]: The meta-study claims that 1 of 1286 HCW wearing a facemask and 119 of 4036 wearing “no facemask” got infected. This is not correct.
According to the study, 78.3% (94/120) of infected HCWs were in fact wearing a surgical mask, and only 20.8% (25/120) did not wear any mask when exposed to the source of infection. The “1 of 1286 HCW” mentioned in the meta-study refers to HCW wearing an N95 (FFP2) respirator, not a medical or cloth mask. - Burke et al. [37]: This study had no results relating to the use of facemasks.
Non-Covid studies were also misinterpreted or misrepresented by the Lancet meta-study authors. For instance, in the case of the non-Covid study with the allegedly biggest impact of masks (Kim et al. [49] about N95 respirators in a hospital with MERS patients), the meta-study authors incorrectly mixed serological and PCR results, again exaggerating the benefit of (N95) masks. The actual results of the Kim et al. study were not statistically significant (p=0.159).
C. Studies relating to “social distancing”
In an additional section, the WHO meta-study evaluated studies on the benefit of “social distancing” measures. However, several independent experts have shown that this section is seriously flawed. The authors again misinterpreted several studies and made several statistical errors.
As with the studies on facemasks, all of these mistakes resulted in falsely claiming or exaggerating a benefit of “social distancing” measures.
For more information on this section, see PubPeer (and links therein) and the CEBM review.
Conclusion
As shown in this analysis, the WHO-commissioned meta-study on the effectiveness of facemasks and social distancing, published in The Lancet, is seriously flawed and should be retracted. Health authorities may want to reconsider their Covid-19 policy guidelines.
Community Use Of Face Masks And COVID-19: Evidence From A Natural Experiment Of State Mandates In The US
https://www.healthaffairs.org/doi/10.1377/hlthaff.2020.00818
Limitations of the Studies Typically Used to Support Masks
- They are all low-level evidence, retrospective observational studies. At the time of my analysis and writing of this paper, none of the studies purporting to support community wearing of masks used high-level randomized clinical trial methodology.
- Cannot distinguish correlation from causation.
-
Does not measure face cover use in the community or any measure of compliance.
- Estimates represent the intent-to-treat effects of these mandates, not the individual-level effect of wearing a face mask in public on one’s own COVID-19 risk.
- Did not measure types of masks worn.
- Did not assess adverse effects of masks.
-
Did not control for other community-wide and hospital-specific interventions that may have contributed to or confounded their observations, including:
- Declarations of emergency (March 10),
- New hospital policies to restrict visitors (March 12) and elective procedures (March 14),
- School closures
- Hospital restrictions on business travel and on-site working (March 16),
- Local public transportation reductions (March 17),
- Issuance of statewide stay-at-home orders (March 24), and
- Automation of screening and testing (March 30).
Masks are Unnecessary
Fear and Politics are Subverting Science and Reason
Public health officials and the media have been warning us that coronavirus kills not just old or immunocompromised people but young people too. While this is true, it remains extremely rare.
A Pandemic of Fraud and Fear is More Dangerous than the COVID-19 Pandemic
Death rate data from the CDC: COVID-19 Pandemic Planning Scenarios
Table 1. Parameter Values that vary among the five COVID-19 Pandemic Planning Scenarios.
Parameters:
- Scenario 5: Current Best Estimate, R0 = 2.5, 40% asymptomatic
- For a definition of R0, see HealthKnowlege-UK (2020): R0 is “the average number of secondary infections produced by a typical case of an infection in a population where everyone is susceptible.” The average R0 for influenza is said to be 1.28 (1.19–1.37); see the comprehensive review by Biggerstaff et al. (2014).
- According to the CDC's latest best estimate, 40% of COVID-19 infections are asymptomatic.
- Parameter values are based on data received by CDC through August 8, 2020.
- These estimates are based on age-specific estimates of infection fatality ratios from Hauser, A., Counotte, M.J., Margossian, C.C., Konstantinoudis, G., Low, N., Althaus, C.L. and Riou, J., 2020
Masking Children in Schools is Unnecessary - So Says The Science
School and daycare transmission studies show that transmission of Covid-19 among unmasked children is remarkably low.
German study finds low Covid-19 infection rate in schools. Tests of pupils and teachers in Saxony suggest children may act as brake on infection.
The study by the University hospital in Dresden analysed blood samples from almost 1,500 children and 500 teachers from 13 schools in Saxony, Germany suggests schools may not play as big a role in spreading the virus as some had feared.
“Of the almost 2,000 samples, only 12 had antibodies,” said Reinhard Berner, a professor of paediatrics at the hospital. In other words, in Saxony’s open and unmasked schools 0.6% of school children demonstrated SARS-CoV-2 antibodies.
All cases were asymptomatic. There were no fatalities.
“Children may even act as a brake on infection,” Berner told a news conference, saying “infections in schools had not led to an outbreak, while the spread of the virus within households was also less dynamic than previously thought.”
“For other states with low infection rates, the study suggests schools could be reopened without fear of causing widespread outbreaks of the virus,” Berner said.
Sweden and Finland: 0.05% of children infected by Covid-19
Sweden kept schools open and unmasked during the pandemic, yet their decision to adhere to the science and do what has always been done before, did not lead to a higher rate of infection among their children compared to neighboring Finland, where schools were closed temporarily.
Based on Covid-19 case data collected from each country during the time period, Feb. 24 to June 14, the percentage of children between the ages of 1-19 infected by Covid-19 was the same:
- Sweden: 1,124 cases 0.05%
- Finland: 584 cases 0.05%
Separate studies by Sweden’s Karolinska Institutet (KI), an independent medical research institute, and the European Network of Ombudspersons for Children and Unicef, showed that Swedish children fared better than children in other countries during the pandemic, both in terms of education and mental health.
COVID-19 transmission rate 0.3% among children in schools and nurseries in New South Wales, Australia
The Lancet Child & Adolescent Health: Effective testing and contact tracing is essential for schools to safely open during COVID-19 pandemic, two studies show. The Lancet; August 3, 2020. https://www.eurekalert.org/pub_releases/2020-08/tl-pss080320.php
Real world data from schools where masks were not required or worn demonstrates a remarkably low rate of transmission of SARS-CoV-2. Analysis of COVID-19 case data from 3103 schools and approximately 4600 nurseries in New South Wales demonstrate that schools and nurseries do not pose a high risk for COVID-19 transmission.
Subset analysis found that only 27 children or teachers went to school while they were infectious, with an additional 18 people later becoming infected. Out of 1448 contacts in total, the rate of secondary transmission was found to be 1.2%.
A subset analysis of 7 schools and nurseries that underwent additional investigations including antibody testing, symptom surveys, and extra RT-PCR testing for the virus showed that the transmission rates among children and staff were extremely low:
- child-to-child rate was 0.3%,
- child-to-staff rate was 1.0%
- staff-to-child rate was 1.5%
- staff-to-staff rate was 4.4%.
The researchers noted that this finding suggests that children are less likely to transmit the virus than adults.
While coronavirus is obviously concerning and a very real threat to some people (namely, the elderly and immunocompromised), these data also show that the risk for the rest of the population is extraordinarily low.
Masks are Harmful: 17 Ways That Masks Can Cause Harm
As a physician and former medical journal editor, I've carefully read the scientific literature regarding the use of face masks to mitigate viral transmission. I believe the public health experts have community wearing of masks all wrong. Here are a few of the mechanisms by which medical masks can be harmful to their wearers and community wearing of face masks is a very bad idea:
Wearing masks for extended periods increased incidences of headaches and negatively affected work performance.
See Jonathan J.Y. Ong, et al., Headaches Associated With Personal Protective Equipment – A Cross‐Sectional Study Among Frontline Healthcare Workers During COVID‐19, Headache, the Journal of Head and Face Pain (May 2020). https://headachejournal.onlinelibrary.wiley.com/doi/full/10.1111/head.13811
1. Medical masks adversely affect respiratory physiology and function.
-
Masks inhibit air flow into and out of the lungs.
- For people with asthma, chronic obstructive pulmonary disease (COPD), and many other chronic lung diseases, face masks are intolerable to wear as they worsen breathlessness.[R]
-
Medical masks lower blood oxygen and raise carbon dioxide such that respiratory rate and depth of breaths are increased.[R]
- Decreasing oxygen and increasing carbon dioxide in the bloodstream stimulates a compensatory response in the respiratory centers of the brain. These changes in blood gases result in increases in both frequency and depth of breaths.
- As masks Increase both the frequency and depth of respirations (breaths), they increase the likelihood that each respiration will contain a larger amount of infectious viral particles. This may worsen the community transmission of CoVID-19 as infected people wearing masks exhale respiratory plumes loaded with greater levels of infectious viral particles. These infectious plumes readily move around the sides, bottom, and top of masks.
- This may also increase the severity of CoVID-19 as the increased tidal volume delivers the viral particles deeper into the lungs.
- These effects are amplified if face masks are contaminated with the viruses, bacteria, or fungi that find their way or opportunistically grow in the warm, moist environment that medical masks quickly become.
2. Medical masks lower oxygen levels in the blood.[R]
Wearing a mask for more than a few minutes causes a significant reduction in a person’s blood oxygen level.
-
Beder, A., U. Büyükkoçak, H. Sabuncuoğlu, Z. A. Keskil, and S. Keskil. 2008. “Preliminary Report on Surgical Mask Induced Deoxygenation during Major Surgery.” Neurocirugia 19 (2): 121–26. DOI: 10.1016/s1130-1473(08)70235-5
- This study of 53 surgeons evaluated the effect of surgical masks on oxygen saturation of hemoglobin in surgeons performing surgery.
- The study revealed the surgeons experienced a significant decrease in the oxygen saturation of arterial pulsations (SpO2) and a slight increase in pulse rates after one hour. The decrease was more prominent in the surgeons over the age of 35.
- Given that a small decrease in SpO2 reflects a large decrease in partial pressure of oxygen in the arterial blood (PaO2)[R], the findings of this study suggests that surgical masks worn more than one hour may lower arterial oxygen enough to induce physiologically detrimental effects.
-
Here are two cases of the tragic consequences of forcing children to wear masks: Two Chinese boys drop dead while wearing face masks during physical exercise classes.[R][R]
Two boys from two Chinese cities died of sudden cardiac arrest within a week. The first boy, 15, collapsed after jogging in PE class while wearing a face mask on April 24. The other boy, 14, reportedly died during a running exam while wearing a mask.
Why would healthy boys drop dead while wearing masks and running in gym class?! To answer this question, we must consider how mask induced deoxygenation and increased oxygen demands of heart muscle during exercise could have precipitated heart attacks in otherwise healthy teenagers:
- Point #1: Heart muscle needs oxygen to survive. And the harder the heart works, the more oxygen it requires. The American Heart Association says this about heart attacks:
- "Your heart muscle needs oxygen to survive. A heart attack occurs when the blood flow that brings oxygen to the heart muscle is severely reduced or cut off completely."[R]
- Point #2: Masks block air intake and decrease arterial oxygen.
Studies of masked individuals have shown that mask wear decreases arterial oxygen. For example, the effects of surgical masks worn by surgeons in the operating room (an environment in which the oxygen blocking effects of masks are minimized by the high air flow, increased oxygen levels, and cool temperature of the operating suite) during major surgery showed a significant decrease in arterial oxygen.[R]
The lesson here is that medical masks should not be worn during intense exercise. As described above and shown in the study of surgeons wearing surgical masks, medical masks block oxygen intake. Depriving the heart of oxygen while exercising, especially intense exercise, could precipitate an acute heart attack.
Any questions? Wait...there’s more...
-
Jogger's lung collapses after he ran for 2.5 miles while wearing a face mask [R]
Mr Zhang's left lung was punctured due to high pressure caused by running. The 26-year-old became breathless whiling jogging with a mask on in China. Doctors said his punctured lung was caused by jogging with a face covering. He is now in stable condition after undergoing an operation, the hospital said.
- Hypoxia increases the risk of blood clot formation.[R]
- Lowering arterial oxygen suppresses the immune system, thus increasing the susceptibility of mask wearers to infectious disease.
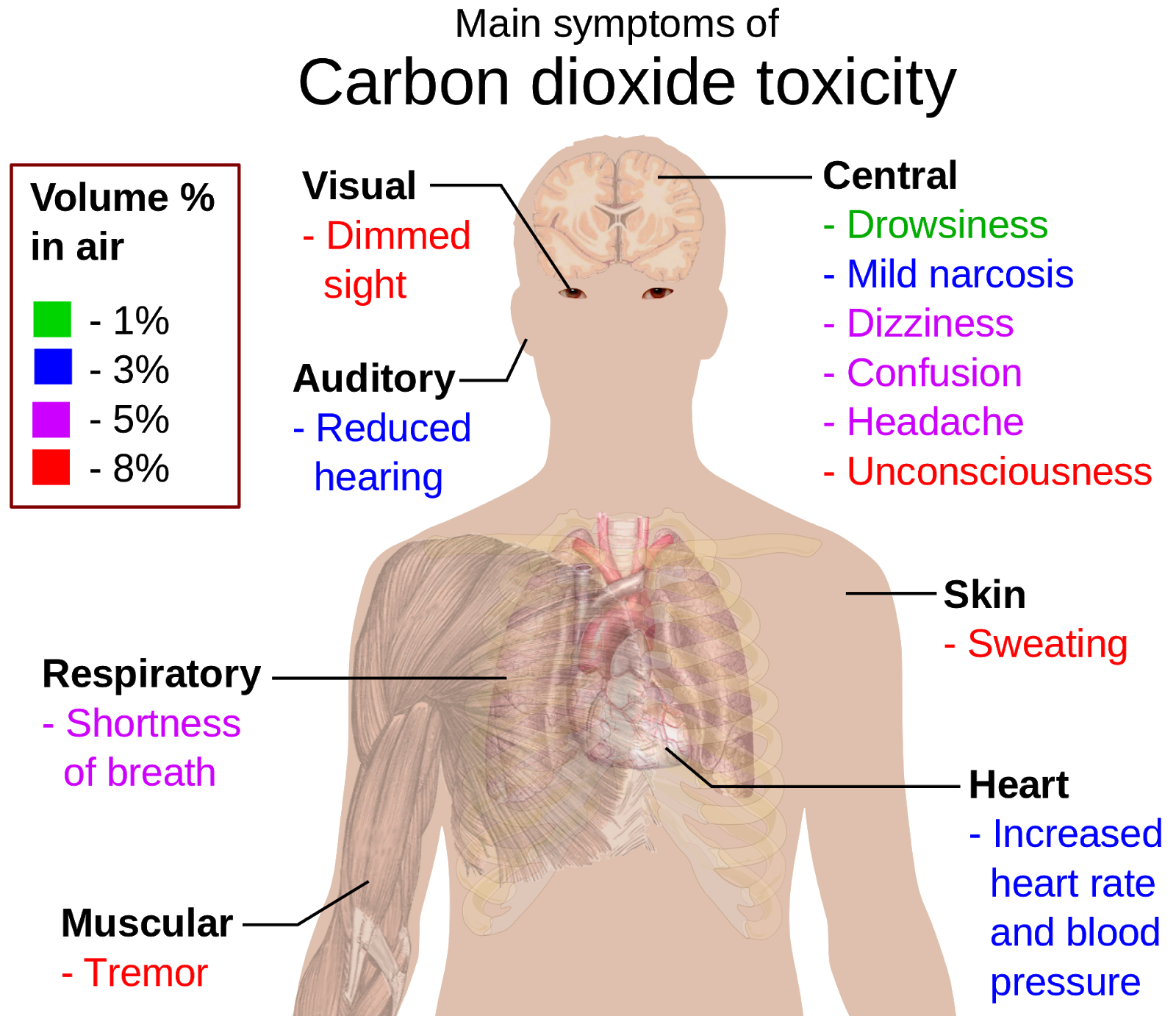
3. Medical masks raise carbon dioxide levels in the blood.
Although the body has robust mechanisms for mitigating transient and minor elevations of CO2 in the air we breathe, these mechanisms can easily be overwhelmed by chronic exposure to significant elevations in CO2, such as occurs with prolonged wearing of a medical mask.
-
The science clearly demonstrates that face masks cause carbon dioxide rebreathing and hypercapnia [R]
- Fletcher, S. J., M. Clark, and P. J. Stanley. 2006. “Carbon Dioxide Re-Breathing with Close Fitting Face Respirator Masks.” Anaesthesia 61 (9): 910. https://onlinelibrary.wiley.com/doi/full/10.1111/j.1365-2044.2006.04767.x
- Exhaled air is rich in carbon dioxide, a waste product of cellular respiration.
- A portion of carbon dioxide previously exhaled is inspired (breathed) at each respiratory cycle.
- Masks trap CO2 rich respiratory exhalations at the mask-mouth interface, force re-breathing of CO2 rich exhalations, raise carbon dioxide blood (CO2) levels. [R]
-
Objective evidence demonstrating how masks increase blood carbon dioxide levels and negatively impact health and function.
- Transcranial Ultrasound Doppler (TCUD) is a noninvasive means of assessing blood flow in the cerebral vasculature. The increase in carbon dioxide partial pressures (PCO2) caused by medical masks can be assessed by TCUD.[R]
- Elevation of PCO2 causes vasodilation of the arteriolar channels leading to a decrease in peripheral vascular resistance. The decrease in peripheral vascular resistance is responsible for the changes in cerebrovascular circulation time, CBF, and the velocity of flow (V) in cerebral arteries.
-
Medical masks force the wearer to inspire (re-breathe) air that is a mix of air from the local environment and the respiratory waste products from the mask wearer’s previous exhalations.
- Respiratory exhalations contain significantly higher levels of carbon dioxide (CO2), one of the waste products of respiration.
- The pulmonary system is designed to collect oxygen and remove CO2 from the body. Masks trap CO2 rich exhalations at the mask-mouth interface.
- Changes in arterial PCO2 considerably influence cranial blood flow (CBF).[R]
- Transcranial Ultrasound Doppler (TCUD) studies on masked and unmasked individuals demonstrate the changes in blood flow in the brain the result from the arterial CO2 elevation that occurs within seconds of donning a mask.
This video demonstrates the use of TCUD and heart rate variability to measure the adverse effects of masking a healthy nine year old child: https://bit.ly/2GGQWiZ
4. SARS CoV-2 is armed with a "furin cleavage site" that makes it more pathogenic.
- The furin cleavage site makes the virus more capable of invading human cells.
- The furin cleavage site makes the virus even more capable of invading cells when arterial oxygen levels decline.[R]
- Therefore, wearing a medical mask may increase the severity of CoVID-19.
5. Medical masks trap exhaled viral (and other) pathogens in the mouth/mask interspace, increase viral/infectious load, and increase the severity of disease.
- Face masks trap exhaled viral particles in the mouth/mask interspace. The trapped viral particles are prevented from removal from the airways. The mask wearer is then forced to re-breathe the viral particles, thus increasing infectious viral particles in the airways and lungs.
- In this way, surgical masks cause self-inoculation, increase viral load, and increase the severity of disease.
-
Neurosurgeon, Russell Blaylock, MD, raises additional concerns:
“By wearing a mask, the exhaled viruses will not be able to escape and will concentrate in the nasal passages, enter the lungs, olfactory nerves, and travel into the brain.”[R]
- Face masks trap exhaled viral particles in the mouth/mask interspace.[R] The trapped viral particles are prevented from removal from the airways. The mask wearer is thus forced to re-breathe the viral particles, increasing infectious viral particles in the airways and lungs. In this way, Medical masks cause self-inoculation, increase viral load, and increase the severity of disease.
-
Asymptomatic or mild cases of CoVID-19 become more severe when the infected is masked, oxygen lowers, viral load increases from particle re-breathing, and the disease overwhelms the innate immune system.
- The main purpose of the innate immune response is to immediately prevent the spread and movement of foreign pathogens throughout the body.[R]
- The innate immune system plays a crucial role in destroying the virus, preventing infection, or decreasing the viral load to decrease the severity of infection.
- The innate immunity’s effectiveness is highly dependent on the viral load. If face masks increase viral particle re-breathing at the same time they create a humid habitat where SARS-CoV-2 remains actively infectious, the mask increases the viral load and can overwhelm the innate immune system.
- This trapping, re-breathing, and increasing pathogen load delivered to the lungs becomes dramatically more dangerous when the medical mask becomes contaminated with the opportunistic viruses, bacteria, and fungi that can grow in the warm, moist environment of the mask.
- “By wearing a mask, the exhaled viruses will not be able to escape and will concentrate in the nasal passages, enter the olfactory nerves and travel into the brain.” - Russell Blaylock, MD
6. SARS CoV-2 Becomes More Dangerous When Blood Oxygen Levels Decline
- Arterial oxygen desaturation is a critical issue in CoVID-19. The virus' ability to infect cells is markedly enhanced by oxygen desaturation, which has been shown to occur even in the ideal operating room environment in which surgeons operate: high air flow/exchange systems, cool temperature, and higher room oxygen levels. when wearing a surgical mask.[R]
- One of the features that make SARS CoV-2 uniquely infectious is the "furin" sequence in the virus that activates increased ACE2 receptor attack and cellular invasion in low oxygen environments.[R]
7. The furin cleavage site of SARS CoV-2 increases cellular invasion, especially during hypoxia (low blood oxygen levels)[R]
- The furin cleavage site found in SARS CoV-2 is the likely result of the bioengineering “gain of function” (which means increasing the virulence of a pathogen) research conducted at the Wuhan Institute of Virology. This unethical, dangerous, and illegal-in-most-countries research is alleged to have been funded by Dr. Anthony Fauci (with $7.4 million taxpayer dollars) and Bill Gates.
- Furin cleavage sites are found in some of the most pathogenic forms of influenza, which can be acted upon by furin and other cellular proteases. The ubiquitous expression of cellular proteases across cell types increases the potential for the virus to successfully infiltrate the host.
- Furin is a membrane-bound protease that is expressed in multiple tissues throughout the human body. Furin is expressed in significant concentrations in the lungs. Thus, viruses in the respiratory tract can make use of this enzyme to convert and activate their own surface glycoproteins. This makes their role in viral protein processing noteworthy.[R]
- Some of the most pathogenic forms of influenza and HIV have similar furin cleavage sites. It is not present in other bat beta coronaviruses. (By the way, Fauci built his career researching and failing to create a vaccine for HIV). The furin cleavage site is NOT present in SARS CoV-1 or MERS, or any of the other known "bat coronaviruses."
- Let me say it again, the SARS-CoV (aka, SARS-CoV-1), which is closely related to the newest SARS-CoV-2 strain, does not bear the furin cleavage site.
So, the question we should all be asking is how did the genetic sequence that codes for this serious gain of function that increases the potential for the virus to successfully infiltrate the host find its way into SARS-CoV-2?
That’s the trillion dollar question; it demands a real and honest answer.
8. Cloth masks may increase the risk of contracting Covid-19 and other respiratory infections.
See MacIntyre CR, Seale H, Dung TC, et al., A cluster randomised trial of cloth masks compared with medical masks in healthcare workers, BMJ Open 2015; 5: e006577, US National Library of Medicine, National Institutes of Health, doi: 10.1136/bmjopen-2014-006577, April 22, 2015. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4420971/pdf/bmjopen-2014-006577.pdf
- “This study is the first [Randomly Controlled Trial] of cloth masks, and the results caution against the use of cloth masks.
- This is an important finding to inform occupational health and safety. Moisture retention, reuse of cloth masks and poor filtration may result in increased risk of infection.”
9. Wearing a face mask may give a false sense of security
- People adopt a reduction in compliance with other infection control measures, including social distancing and hands washing.[R]
10. Masks compromise communications and reduce social distancing
- The quality and volume of speech between two people wearing masks is considerably compromised and they may unconsciously move closer to improve communications
- This increases the likelihood of becoming exposed to the infectious viral particles in the respiratory plumes of aerosolized droplet nuclei that escape the top, bottom, and sides of the masks.
11, Untrained and inappropriate management of face masks:
- The public is untrained and inadequately educated in the proper selection of masks (most are wrongly wearing cloth masks), proper wear, sterility management, and importance of not reusing single use masks.
- People must not touch their masks, must change their single-use masks frequently or wash them regularly, dispose of them correctly and adopt other management measures, otherwise their risks and those of others may increase.[R][R]
- We can all observe the countless ways in which people in communities are mis-wearing, mishandling, and increasing their own and the communities risk of contracting infectious disease, including CoVID-19.
12. Masks Worn Imperfectly Are Dangerous
To fully appreciate the danger of improper wear and handling of face masks, all you have to do is observe how the public is managing them. Take a trip to Walmart or your local school and observe how mask wearers pull masks from their pocket or purse, drop the masks on the floor, cough and sneeze in them, move them below the nose, on their heads, or under their chin. I see it every day. I also see their soiled and stained surgical face masks and know that these people are dangerously reusing a mask that should never be reused.
You don’t need a clinical trial to determine that even when mask-wearers manage to don a fresh, sterile mask properly, keep them on for more than a few minutes at a time, they very quickly contaminate the mask, their environment, and increase their risk of infection as the mask induces them to compulsively touch their faces and their masks.
- The World Health Organization, which has repeatedly changed its position on universal masking, is adamant that if face masks are not worn carefully, correctly, and kept sanitary, they are worse than ineffective.
-
In other words, masks worn imperfectly are dangerous.
- See Linda Lacina, WHO updates guidance on masks for health workers and the public - here's what you need to know, World Economic Forum (June 5, 2020). https://www.weforum.org/agenda/2020/06/who-updates-guidance-on-masks-heres-what-to-know-now/
People can infect themselves if they use contaminated hands to adjust a mask or repeatedly take it on or off,” explained WHO Director-General, Dr Tedros Adhanom Ghebreyesus. "I cannot say this clearly enough. Masks alone will not protect you from COVID-19."
Failing to follow strict medical standards for wearing protective equipment and specification of sterilizing and cleaning often leads to “skin and mucous membrane injury, which may cause acute and chronic dermatitis, secondary infection and aggravation of underlying skin diseases.”
- Yan, et al., Consensus of Chinese Experts on Protection of Skin and Mucous Membrane Barrier for Health-Care Workers Fighting against Coronavirus Disease 2019. Dermatologic Therapy, March 2020, e13310. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7228211/pdf/DTH-9999-e13310.pd
i Witness NEWS
The Truth Never Suffers from Honest Examination!